Spinal implants have significantly improved outcomes for patients with conditions like degenerative disc disease, spinal instability and scoliosis. However, their long-term success can vary based on the type of implant, surgical technique and individual patient factors. Dr. Larry Davidson, an experienced specialist in spinal care, emphasizes the growing role of Artificial Intelligence (AI) in optimizing these outcomes. By analyzing patient-specific data and real-world evidence, AI enables surgeons to move beyond short-term solutions and make informed decisions that support long-term implant performance and patient well-being.
By using machine learning algorithms to analyze large datasets, AI tools can simulate and compare the expected performance of different spinal implants over time. This helps surgeons make better-informed choices before surgery and allows patients to understand what kind of outcomes they can realistically expect. With predictive modeling at the center of implant planning, spine care is becoming increasingly data-driven, customized and forward-thinking.
Why Long-Term Implant Performance Matters
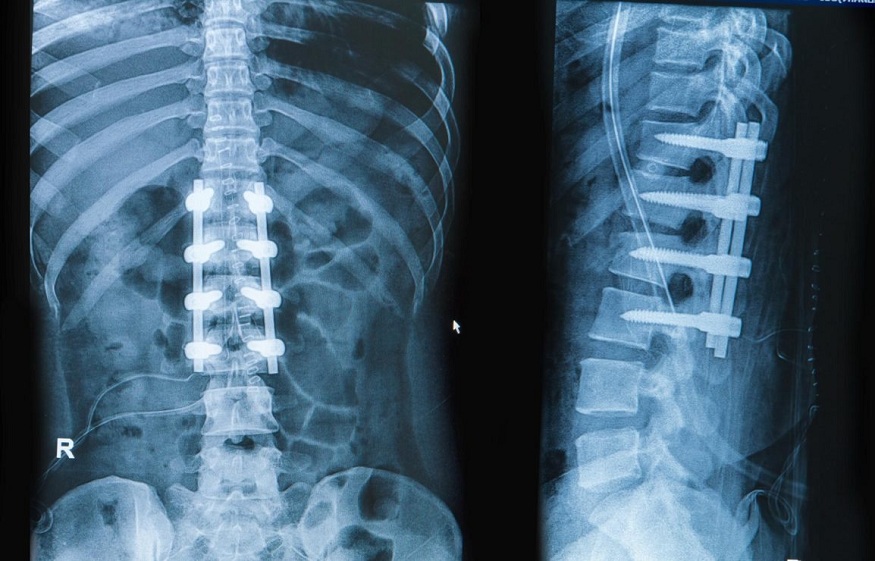
While the immediate success of spinal surgery is often measured by pain reduction and mobility, the long-term value of an implant lies in its durability, integration with the spine and compatibility with the patient’s daily life. Poor implant selection can result in complications like loosening, wear, adjacent segment disease or the need for revision surgery, sometimes years after the initial procedure.
How AI Models Implant Behavior Over Time
Predictive models use historical data from thousands of prior implant cases, often drawn from global surgical databases and long-term clinical studies. These datasets include factors like:
- Implant type and material (e.g., titanium vs. polymer)
- Patient demographics and health profile
- Surgical approach and hardware positioning
- Postoperative recovery patterns
- Long-term complications or failures
Supporting Implant Selection Before Surgery
One of the most practical applications of AI modeling is during the preoperative planning stage. When selecting between implant options, such as artificial discs, rods, screws or cages, AI models offer forecasts for each choice based on patient data.
If the system predicts a higher likelihood of long-term success with a particular implant type, that recommendation becomes part of the shared decision-making process. This level of clarity not only improves surgical strategy but also boosts patient confidence in the selected treatment path.
Dr. Larry Davidson explains, “Emerging minimally spinal surgical techniques have certainly changed the way that we are able to perform various types of spinal fusions. All of these innovations are aimed at allowing for an improved patient outcome and overall experience.” When paired with AI-driven forecasting, these techniques support a more personalized and informed approach to implant selection.
Modeling Biomechanical Stress and Fatigue
Over time, spinal implants are subject to wear and biomechanical forces. Walking, lifting, twisting and even subtle postural deviations can stress the hardware and the surrounding bone. AI tools can simulate these forces using the patient’s posture data, gait analysis and physical activity level.
This modeling helps estimate how an implant will age, whether it will maintain stability, cause stress shielding or lead to hardware fatigue. If the predicted wear-and-tear risk is high, the surgical team might opt for reinforced fixation or choose a different material altogether.
Forecasting Adjacent Segment Disease
A well-documented issue in spinal fusion cases is Adjacent Segment Disease (ASD), where the levels above or below the fusion site experience increased stress and degeneration. AI models can simulate the likelihood of ASD by evaluating spinal biomechanics before and after implant placement.
These predictions help surgeons make informed decisions about the number of levels to fuse, whether to use motion-preserving devices like artificial discs, or how to tailor the patient’s post-op therapy plan to minimize stress on adjacent levels.
Postoperative Monitoring and Refinement
AI modeling doesn’t end in the OR. Post-surgery, the same systems can be used to track implant performance through imaging, wearable device data and patient-reported outcomes. If early signs of implant wear, misalignment or stress are detected, the system can prompt clinicians to intervene early, potentially avoiding larger issues down the road.
In cases where long-term modeling predicts increased complication risk, patients may be scheduled for more frequent imaging or advised on specific movement restrictions and strengthening programs.
Helping Patients Understand Their Options
AI’s ability to simulate long-term outcomes also benefits patient education. Through visual tools and comparative charts, patients can see how different implants may affect their mobility, pain levels and lifestyle over time. For example, one implant might allow for greater post-op flexibility, while another offers enhanced structural stability.
This clarity helps patients make decisions aligned with their personal goals, whether they prioritize returning to sports, reducing recovery time or minimizing future surgeries.
Enhancing Innovation in Implant Design
Manufacturers and researchers can also use AI modeling to improve implant design. By inputting performance data from earlier implant designs into machine learning models, developers can pinpoint failure points, refine shapes and materials and engineer more adaptable, long-lasting devices.
As data drives design and better design improves results, patients receive safer, more durable implants that fit their anatomy and needs more precisely.
Ethical Use and Model Validation
As with any predictive tool, transparency and validation are essential. Models must be trained in diverse, representative datasets to ensure accuracy across different populations. Surgeons should be able to understand how the model reached its recommendations and verify that those conclusions match real-world trends.
AI modeling should support, not replace, clinical decision-making. The ultimate choice still rests with the surgeon and patient, guided by context, experience and goals.
A Long-Term Vision Made Smarter
The decision to place a spinal implant is more than a surgical choice. It represents a long-term investment in a patient’s mobility, comfort and quality of life. Predictive modeling helps ensure that investment is guided by data, offering insight into how different implants are likely to perform over time.
With AI supporting planning, monitoring and follow-up care, spine surgery is becoming more precise and patient-specific. These tools give providers the ability to anticipate complications, tailor treatment strategies and support outcomes that last well beyond the initial procedure.
The Future of Implant Optimization
AI modeling will likely become even more personalized. As these systems integrate genetic data, motion sensors and robotic surgical tools, implant planning will become even more customized. 3D-printed devices tailored to each patient’s anatomy are already in development, with AI helping predict how they’ll perform over the long term.
Spinal surgeries may soon include simulations that factor in anatomy, motion, lifestyle and long-term function, helping tailor implants for lasting success.